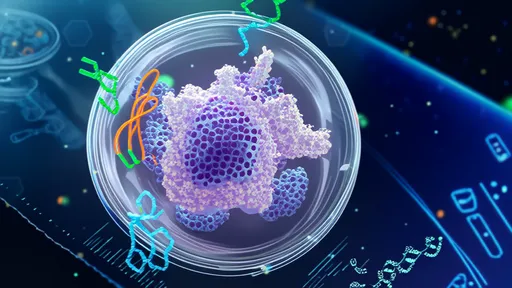
The human body's immune system is a marvel of biological engineering, capable of defending against countless pathogens. Yet sometimes, this intricate defense mechanism turns against itself, leading to autoimmune diseases like rheumatoid arthritis, Crohn's disease, or lupus. Traditional treatments often involve suppressing the entire immune system, leaving patients vulnerable to infections. Now, a groundbreaking approach merging neuroscience and immunology – vagus nerve decoding through electronic pills – promises to revolutionize autoimmune therapy.
At the heart of this innovation lies the vagus nerve, the longest cranial nerve that serves as a superhighway between the brain and major organs. Recent research reveals this nerve doesn't just regulate heart rate and digestion – it plays a crucial role in controlling inflammation through what scientists call the "inflammatory reflex." When this neural circuit malfunctions, it may contribute to the uncontrolled inflammation seen in autoimmune disorders. Electronic pills designed to interface with the vagus nerve could restore this critical communication pathway.
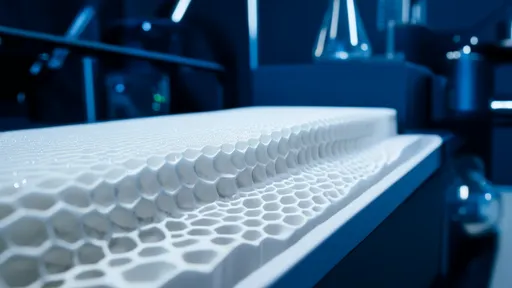
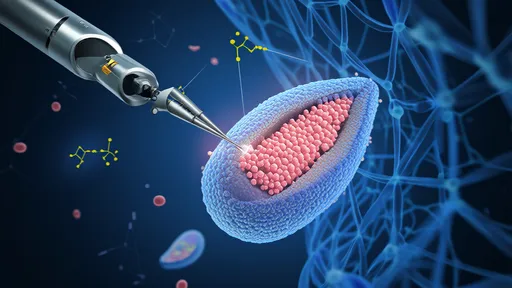
The concept of bioelectronic medicine isn't entirely new, but the development of swallowable electronic pills represents a quantum leap forward. Unlike implanted nerve stimulators that require surgery, these smart pills travel through the digestive tract while wirelessly communicating with external devices. As they pass near vagus nerve branches in the gut, they deliver precisely calibrated electrical pulses that appear to "reset" abnormal immune responses. Early clinical trials show remarkable precision – the devices can distinguish between normal digestive activity and pathological inflammation patterns.
What makes this approach particularly exciting is its potential for personalization. Each patient's vagus nerve signals create a unique "inflammatory fingerprint" that electronic pills can learn to interpret. Machine learning algorithms analyze these neural patterns in real-time, adjusting stimulation parameters to individual needs. This stands in stark contrast to conventional immunosuppressants that take a one-size-fits-all approach, often causing severe side effects when dosage guesses miss their mark.
The implications extend beyond autoimmune conditions. Researchers speculate that properly decoded vagus nerve signals might help treat other inflammation-driven diseases like Alzheimer's, diabetes, and even depression. The nerve's extensive connections throughout the body make it a promising target for addressing multiple conditions simultaneously. Some trials have reported unexpected improvements in comorbid conditions when patients received vagus nerve stimulation for their primary autoimmune diagnosis.
Despite the enthusiasm, significant challenges remain. The vagus nerve's complexity means scientists are still mapping its numerous functions and connections. There's also the question of long-term effects – while early results show sustained benefits after treatment courses, the medical community awaits data on decade-long usage. Regulatory hurdles present another obstacle, as current frameworks struggle to classify these hybrid devices that blur the line between pharmaceuticals and medical hardware.
Ethical considerations have emerged alongside the technology's advancement. The ability to modulate neural activity raises questions about identity and autonomy. Could altering vagus nerve signals change aspects of personality or emotional responses? Research suggests the stimulation parameters used for inflammation control don't affect mood, but the philosophical debate continues. Patient advocacy groups emphasize the importance of informed consent, especially for treatments interacting with the nervous system.
Looking ahead, the convergence of neurology, immunology, and bioengineering appears poised to transform autoimmune care. Pharmaceutical companies are investing heavily in "electroceuticals," with several electronic pill prototypes nearing FDA review. If successful, this approach could shift the treatment paradigm from broadly suppressing immunity to precisely retraining it – offering hope to millions for whom current therapies fall short. The vagus nerve, once viewed primarily as a passive messenger, may hold the key to unlocking a new era of personalized, neuromodulatory medicine.

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025

By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025
By /Jul 18, 2025

By /Jul 18, 2025